- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- ¿Está enfermo su hijo?
- Parent Resources
- The Connection Journey
- Calma Un Bebé Que Llora
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Política y procedimientos en el hospital
- Preguntamos Porque Nos Importa
-
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Mental Health Town Hall
martes, 23 de abril de 2024Join Children’s Hospital Colorado pediatric experts for a virtual...
-
Research & Innovation
- Overview
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.


Adult Congenital Heart Disease Patient Care
Written by Joseph Kay, MD
History of adult congenital heart disease
Despite decades of refining the diagnosis and intraoperative and postoperative care for congenital heart patients, mortality remained high for many complex congenital heart lesions — above 25% for neonates and infants until the 1990s. After the mid-1990s, mortality dropped to less than 5% for this young population5. With this dramatic improvement in care over the last two decades, the number of survivors with complex congenital heart disease who are reaching adulthood has rapidly increased. Now, there are more adults than children with moderate and complex congenital cardiac defects6.
Setting standards of care for adults living with congenital heart defects
Few of these adults can be considered cured, with most having a higher mortality compared to age-matched controls7. Lifelong care of adult congenital heart disease (ACHD) survivors by experts in congenital heart disease, therefore, remains important. A milestone population study has shown that patients with ACHD in the care of ACHD specialty centers had lower mortality than those cared for by non-ACHD specialty centers8.
Variation in practice patterns between ACHD centers throughout the United States raised concerns that not all programs may be providing care comparable to international centers involved in the milestone study. In an effort to set minimum standards of care for ACHD centers across the country, the Adult Congenital Heart Association, a patient advocacy nonprofit organization, in partnership with ACHD specialists, has developed an accreditation program for ACHD centers setting a minimum standard of care.
Children's Hospital Colorado's Adult Congenital Heart Disease Program spans both Children's Colorado and the University of Colorado Hospital. Our Program was honored to serve as one of the pilot programs for this accreditation process and is one of 24 programs to receive comprehensive care center accreditation. It remains the only program in Colorado.
Adults receiving care from ACHD experts
With the rapid growth of this population, combining both the complexity of congenital heart abnormalities along with adult onset medical problems, the American Board of Medical Specialties (ABMS) developed a new subspecialty of adult congenital heart disease. The first board exam was offered in 2015. Through 2019, cardiologists from either a pediatric cardiology or an adult cardiology background with experience in caring for these patients have been eligible for this board certification. After 2019, board eligibility requires an additional two-year advanced fellowship in adult congenital cardiology after either a pediatric or adult cardiology fellowship. Our Program was one of the first five of such training programs to receive accreditation from the accrediting council for graduate medical education. Currently 20 of these programs exist across the country.
More than 60% of adult survivors with congenital heart disease are not in the care of congenital heart disease experts in the U.S., which has been shown to lead to increased mortality and preventable morbidity.
There are many reasons why these adults are being lost to care:
- First, many survivors and their physicians are unaware of the presence of these specialized ACHD care providers and programs and their impact on outcomes.
- Secondly, many believe they were "fixed" with their surgery as a child (sometimes mistakenly told so by their pediatric cardiac surgeon or cardiologist). They are not aware they should continue to receive lifelong care, let alone lifelong care from an adult congenital expert.
When problems arise, survivors understandably believe that any adult-trained cardiologist or cardiac surgeon can treat their issues. While this is true for some, most adult-trained cardiologists and cardiac surgeons are not familiar with the variety of cardiac issues that may be present for a specific lesion, and often fail to treat all the issues.
Missed opportunities for providing proper ACHD care
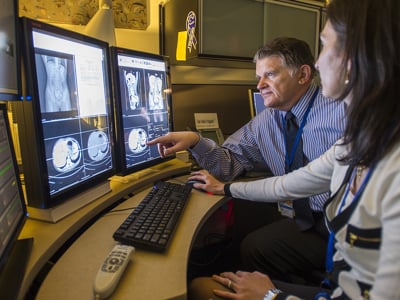
A common example of missed opportunities for addressing comprehensive care for these patients who are lost to follow-up are those who develop new-onset arrhythmia and then seek care. Arrhythmias are a common problem that cardiologists and electrophysiologists deal with in non-congenital heart survivors in most communities. Most physicians are quite capable of treating these arrhythmias in the non-congenital population, which may involve performing an ablation or placing an automatic implantable cardiac defibrillator.
What physicians are not usually familiar with is the unique variations of ACHD patients' hearts that alter the approach to such procedures, let alone addressing underlying, otherwise asymptomatic hemodynamic issues that frequently are at least partially responsible for the development of these arrhythmias. Chronic heart volume loading from severe valve regurgitation drives more electrical changes in the heart, and if left untreated, will ultimately lead to chronic congestive heart failure.
While most adult community cardiologists are familiar with such problems in normally developed hearts, they are not as familiar in recognizing and understanding the unique approaches developed to evaluate and treat these problems in congenital heart patients. Failure to address all these issues (usually not done in outside congenital centers) will lead to more recurrent arrhythmias and permanent heart failure.
Current advanced treatment options for ACHD patients
With recent advances, fewer of these patients will require repeat open-heart surgery. New transcatheter therapies have been developed that may make it possible for less than half of pulmonary valve replacement procedures to have to be done surgically — decreasing morbidity and anxiety for many patients. If surgery is needed, it has been shown that when congenital heart surgeons perform the surgery, such as in our Program, mortality is much lower.
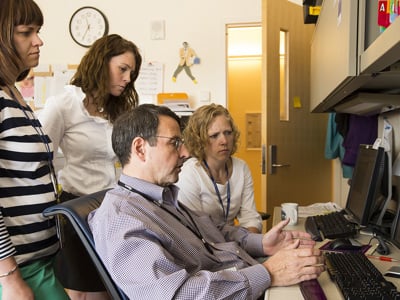
With over 300 ACHD board-certified physicians in the U.S., Children's Colorado has recruited and retained seven physicians trained in the care of these complex ACHD patients. This allows us to provide specialized care for ACHD patients throughout our seven-state region.
We have been able to develop clinics at both Children's Colorado and University of Colorado Hospital five days per week, in addition to outreach clinics in Montana, Wyoming and Colorado. The goal of these clinics is to remove barriers to specialty care and bring ACHD survivors back into care, maximizing long-term health and the highest possible functional status.
Sources:
- Gross RE. Surgical Management of the Patent Ductus Arteriosus: With Summary of Four Surgically Treated Cases. Ann Surg 1939;110:321-56.
- Crafoord C. Classics in thoracic surgery. Correction of aortic coarctation. Ann Thorac Surg 1980;30:300-2.
- Blalock A. The technique of creation of an artificial ductus arteriosus in the treatment of pulmonic stenosis. J Thorac Surg 1947;16:244-57.
- Kirklin JW, Dushane JW, Patrick RT et al. Intracardiac surgery with the aid of a mechanical pump-oxygenator system (gibbon type): report of eight cases. Proc Staff Meet Mayo Clin 1955;30:201-6.
- Khairy P, Ionescu-Ittu R, Mackie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol 2010;56:1149-57.
- Gilboa SM, Devine OJ, Kucik JE et al. Congenital Heart Defects in the United States: Estimating the Magnitude of the Affected Population in 2010. Circulation 2016;134:101-9.
- Verheugt CL, Uiterwaal CS, van der Velde ET et al. Mortality in adult congenital heart disease. Eur Heart J 2010;31:1220-9.
- Mylotte D, Pilote L, Ionescu-Ittu R et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation 2014;129:1804-12.



 720-777-0123
720-777-0123