Kids with pulmonary hypertension face a real risk of a cardiac event every time they undergo catheterization. And yet cath is currently the reference standard to monitor the progress of their disease. At Children's Hospital Colorado, a cadre of researchers is working to adapt MRI to that task — and they're seeing the heart in a way it's never been seen.
The risks of catheterization for monitoring pulmonary hypertension
Pediatric cardiac interventionist Jenny Zablah, MD, straps on a lead vest. Her patient, 2-month-old Marcus *, lies anesthetized in the Cath Lab. An access sheath is placed in his femoral artery and vein. The catheters are fed through. Soon they appear in the monitor above him, one in the aorta, one in the pulmonary artery.
Six weeks premature, Marcus was born with a large patent ductus arteriosus that failed to close. In a healthy baby, pulmonary blood pressure should be about a third of systemic pressure. Marcus's open PDA lets the pressures in the pulmonary artery and the aorta equalize. Today's mission: Get a read on Marcus's pulmonary hypertension and see if Dr. Zablah can safely close the PDA.
"This is a low-complexity case," Dr. Zablah remarks, "but many of our PH patients are very sick. Anesthesia makes the systemic blood pressure drop, so they're at high risk to go under sedation. Sometimes they go into cardiac arrest."
"For every cath procedure these kids get, the chance of a catastrophic event is 3.3%," says pediatric cardiologist Uyen Truong, MD. "But a lot of kids need it serially, over a lifetime. So you can imagine the risk."
Leveraging cardiac MRI to image the heart
Dr. Truong and bioengineer Michal Schafer, PhD, talk cases. On their agenda: a patient with idiopathic pulmonary arterial hypertension, a rare subset of PH, who had pressures so dire surgeons shunted his pulmonary artery to the descending aorta to give his lungs a way to offload pressure. The need to know his status is urgent and constant. He's had several cath procedures.
A day after his last one, he also got an MRI. For the patient, and for most of the people in the room, it wasn't much different from any other scan.
"MRI excites hydrogen," says Dr. Schafer. "Anywhere there's hydrogen, such as in water, you can excite that atom and get a signal. Then you can map the location of those signals, that's how you get the overall image."
"Typically you're exciting a slice," adds Nivedita Naresh, PhD, a bioengineer in the Advanced Imaging Lab specializing in MRI pulse sequence programming. "The difference here is that we're exciting a volume."
That's trickier than it sounds. It changes the pulse sequence programming, which tells the scanner how to gather data, and the processing, which sorts it into a meaningful image. It's even trickier when the sequences run continuously to produce a moving image of blood-flow in an organ constantly in motion.
The sequences Dr. Naresh is working on compensate for that by gating to ECG, essentially syncing to the heart's natural rhythm. But even then, there's no commercial software that can process the data they generate. For that, Dr. Schafer uses code he helped develop.
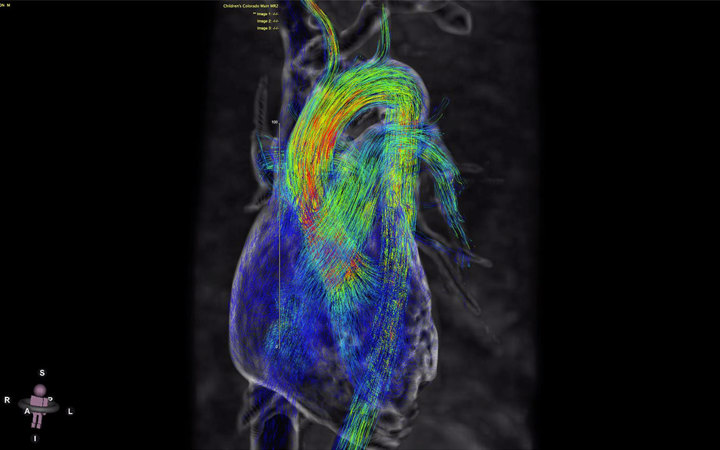
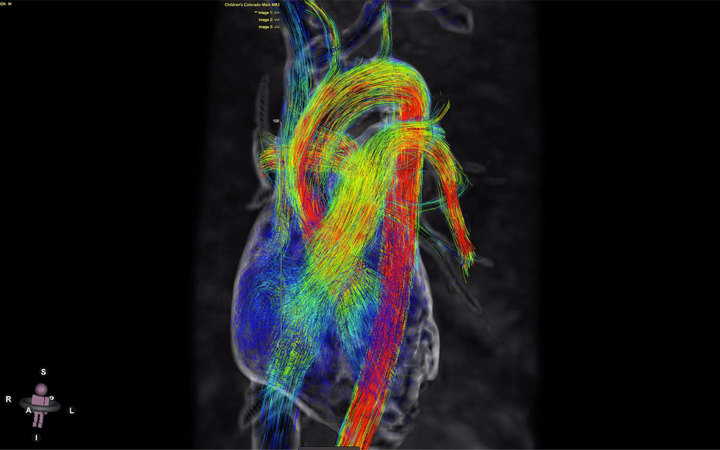
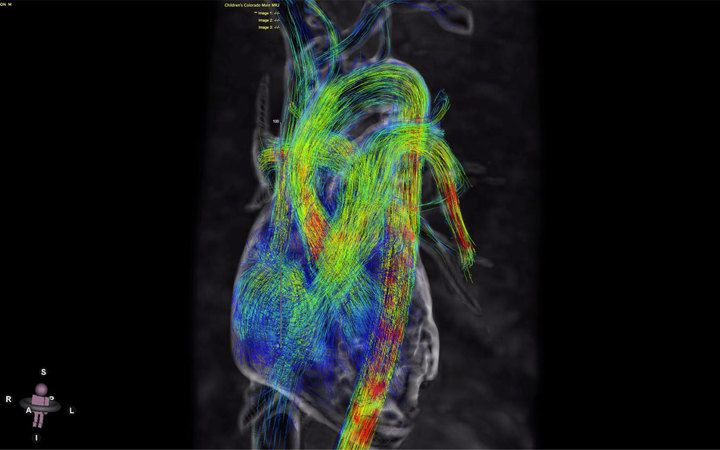
The result is 4D MRI: images of the heart in three dimensions, over time.
"Here's where the magic happens," he says.
The heart in four dimensions
On his screen, Dr. Schafer pulls up the rough shape of his patient's heart. Rendered in sinews of color, it comes alive with a click: A rush of green pours into the pulmonary artery and then the aorta, the irregular flows of the shunt breaking up into sprays of blue. Each line represents a direction of flow. Each color represents a velocity. From this dashboard, he and Dr. Truong can get a read on most of the information a cath provides. But they're seeing much more than that.
Dr. Schafer rotates the view and points to where the shunt empties into the aorta. "You can see all these spirals and vortices here. The shunt is helping the heart pump less against pressure, but the system is not designed to convey flow in this fashion. Dr. Truong said, 'Let's check the descending aorta.' Well voilà, we find there is some stiffening there."
"We've never been able to see that before," adds Dr. Truong. "We're putting together the first case report on this. When I presented it, people were blown away."
What they've seen is so novel, so groundbreaking, in fact, that Dr. Truong's group has published 15 papers in the last two years alone. Their National Institutes of Health-funded comparison study of catheterization and 4D MRI in patients with pulmonary arterial hypertension, like the one on their screen, just finished its first of five years.
So far, signs are promising that MRI data correlate with conventional cath data. It's faster, cheaper and safer, all with no radiation, no risk and no downtime.
"This technology lets us understand the physics of pulmonary hypertension better than we ever have," says Dunbar Ivy, MD, Chief of Pediatric Cardiology. "We're not there yet, but it's possible it will help us pick treatment options to improve flow characteristics in these patients lifelong."
Building a better MRI sequence
One advantage of 3D scanning is that a volume contains more signal than a plane, which maximizes the signal-to-noise ratio — meaning cleaner, higher-resolution images. The challenge is that more signals mean more data, and that means more time in the machine.
"We're going under the hood of the scanner and redesigning how it obtains this data," says says bioengineer Alex Barker, PhD, Director of the Advanced Imaging Lab.
To do that, he and Dr. Naresh, who cut her teeth programming Seimans machines, are applying techniques similar in concept to file compression in computing. Building algorithms that account for known sparsity, they are training the machine not only to minimize the time of data acquisition, but also to enable scanning in patients of minimal size.
Essentially a 3D pixel, a voxel is a scanner's most basic unit of meaning. A neonate's aorta might measure 10mm across. The sequence needs at least five voxels in that volume to extract meaningful information — and currently, there's no way to measure with that kind of precision. But Dr. Naresh is working on it.
"We're pushing the limits of the sequence," says Dr. Truong.
A new measure of exercise physiology
Using those sequences, Dr. Truong and her team are also able to measure the limits of their patients' disease physiology in ways they've never been able to before. Particularly in a cardiopulmonary disease like PH, exercise physiology can reveal underlying markers of disease that resting physiology keeps hidden.
But you can't get exercise physiology with cath. You could put a kid on a treadmill and then do an echocardiogram right afterward, but by then you're not really getting maximum exercise physiology. The heart rate drops. Pressures decrease.
With 4D MRI, Dr. Truong's team sticks an exercise bike right in the machine.
Currently, there's only one commercially available exercise bike for MRI. "And you basically have to buy a crane because it weighs about 200 lbs.," says Derek Eilers, MS, Principal Engineer of Montview Biomedical Design and frequent Children’s Colorado collaborator.
Eilers, a former bike racer who honed his chops designing fitness equipment, figured he could do better.
The first challenge, he knew, would be to build it entirely out of non-ferrous components that wouldn't interfere with the machine. The second would be to construct a design that could work for kids and adults of a wide range of heights in a narrow tube.
The design he came up with utilizes an elliptical path to maximize knee clearance. It transmits signals via Bluetooth to eliminate artifacts, and it measures resistance, power and cadence. It also weighs just 40 lbs.
The far-ranging treatment implications of 4D MRI
Meanwhile, Dr. Barker, a key player in the development of 4D MRI, is using the technology to study complex hemodynamics in vascular disease, specifically in neurovascular malformations where blood short circuits from the arterial to the venous system without traveling through capillary beds. Those can have devastating consequences for the patient, but they're also difficult to localize, impossible with conventional MRI. Dr. Barker's sequences can help map those connections — a potentially lifesaving planning tool that surgeons can use to seal them off.
"You can't do this with any other imaging technique," he says.
"We're using it in a number of studies," says pediatric endocrinologist Kristen Nadeau, MD, MS. "We want to detect early disease in youth with diabetes, but we're not going to cath or do something invasive. We've already used this to uncover some signs of vascular disease that weren't detectible by less sensitive methods."
One such study looked at markers of stiffness and compliance in the aorta of 50 kids with type 1 diabetes and found that metformin could improve vascular stiffness over time. Given that metformin doesn't improve blood sugar control in type 1 diabetes — and thus isn't currently included in the typical treatment regimen — that finding stands to change the standard of care.
Dr. Nadeau and her group recently published that in Circulation, and they're starting to apply the technology in type 2 diabetes populations.
And on Dr. Truong's side, her team of cardiologists, radiologists, bioengineers and computer scientists is working to apply 4D MRI on a smaller scale.
Because neonates are at even higher risk for cath, the main disease tracking tool tends to be echocardiogram — the limitations of which can render its information imprecise. Reliable 4D images could change the care landscape for newborns with PH and related conditions like bronchopulmonary dysplasia. But the implications of that capability extend far beyond the heart.
"One day," says Dr. Ivy, "this is going to be ubiquitous."
* Patient information changed to protect privacy
Featured Researchers

Jenny Zablah Alabi, MD
Interventional cardiologist
The Heart Institute
Children's Hospital Colorado
Associate professor
Pediatrics-Cardiology
University of Colorado School of Medicine
Michal Schafer, PhD
Clinical instructor
Surgery-Cardiothoracic
University of Colorado School of Medicine
Uyen Truong, MD
Pediatric cardiologist
Children's Hospital Colorado





 720-777-0123
720-777-0123