- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Click to find the locations nearest youFind locations by region
See all locations -
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Public Meeting: 2024 Community Benefit and Hospital Transformation Program
Tuesday, May 14, 2024Join Children's Hospital Colorado at one of our virtual events to learn...
-
Research & Innovation
- Overview
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.


Food Protein-Induced Enterocolitis Syndrome (FPIES): An Often-Overlooked Food Allergy
Written by Dan Atkins, MD
Children with an immunoglobulin-E (IgE)-mediated food allergy present with symptoms typically associated with allergic reactions that occur within minutes to hours after ingestion of the culprit food and have a positive skin test to the offending food. In contrast, children with non-IgE-mediated food allergies often present with symptoms isolated primarily to the gastrointestinal tract such as abdominal pain, nausea, vomiting, diarrhea, food refusal and failure to thrive.
Providers may miss or delay the diagnosis of non-IgE-mediated food allergy early in life due to the overlap of symptoms with other GI disorders, a longer delay between food ingestion and symptom onset, a lack of biomarkers (prick skin tests are usually negative) and poor awareness of these conditions.
Food protein-induced enterocolitis syndrome (FPIES) is a perfect example of a non-IgE-mediated food allergy that is often misdiagnosed or not diagnosed in a timely fashion. FPIES presents during infancy in both acute and chronic forms.
The acute form of FPIES occurs either after initial food introduction or upon reintroduction following removal of a culprit food from the diet. Symptom onset typically occurs within two to four hours of food ingestion and consists of repetitive, profuse vomiting in addition to pallor and lethargy, often followed hours later by diarrhea. Severe reactions result in acute dehydration, hypotension and/or bloody, mucousy stools filled with eosinophils and leukocytes. Peripheral blood neutrophil counts are increased and often accompanied by thrombocytosis.
Symptoms of FPIES
Because of the acute onset of symptoms, children with FPIES are often seen urgently in their doctor's office or in the emergency department. There, they are frequently misdiagnosed with suspected sepsis, acute viral gastroenteritis or surgical conditions, further delaying the correct diagnosis.
In contrast, chronic FPIES occurs when the culprit food is introduced early in life and fed regularly, such as milk or soy formula. Symptom onset is usually within the first three months of life and between one to four weeks of formula introduction. Onset can occur later if formula introduction is delayed, but rarely occurs after 1 year of age.
Classic symptoms include persistent irritability, abdominal distention, lethargy, failure to thrive and bloody diarrhea accompanied by laboratory findings of metabolic acidosis, neutrophilia, eosinophilia, anemia and hypoalbuminemia. Methemoglobulinemia and acidosis have been reported in up to a third of infants with severe reactions. Removal of the offending food from the diet results in significant improvement over the following 24 to 48 hours, although symptoms return acutely following subsequent exposures.
Causes of FPIES
Milk and soy formulas are the most common causes of FPIES, and in the United States, about half of the children who react to one also react to the other. Foods that often trigger solid food FPIES include several that rarely cause IgE-mediated reactions. They are commonly the first foods introduced into the infant diet, which is another reason that food allergy is rarely considered the cause. For example, rice is the most common cause of solid food FPIES while other common triggers include oat, barley, avian meats, sweet potato, white potato and corn.
A relatively common scenario for FPIES is the infant who is fed rice cereal for the first or second time and develops classical FPIES symptoms two to four hours later. Because rice is not considered a common food allergen, the diagnosis of a food allergy is not considered or is even discounted if suggested by a parent. About a third of the children with FPIES to milk and/or soy subsequently develop FPIES to solid foods, whereas about 80% of infants with solid food FPIES react to more than one food.
High-risk food groups in the first year of life include grains, legumes and poultry. Fortunately, most children outgrow milk and soy FPIES by 3 years of age, although resolution of solid food FPIES may take longer. Interestingly, FPIES to fish and shellfish has been described in older children and adults.
Diagnosis of FPIES
Knowledge of the common food triggers, typical symptoms, timing of symptom onset following food exposure and the different forms of FPIES (acute and chronic) is critical to making the diagnosis. Allergen skin testing is usually negative although recent evidence suggests that those with positive skin tests take longer to outgrow FPIES and may subsequently develop IgE-mediated food allergy. Occasionally, an oral food challenge to the suspected food after a period of avoidance is necessary to confirm the diagnosis. Oral food challenges are also considered after 12 to 18 months without a reaction to determine whether the child has outgrown FPIES to the incriminated food.
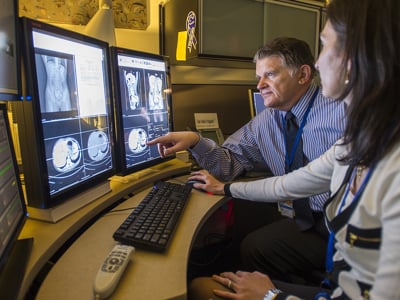
Because approximately half of positive challenges result in repetitive vomiting and acute dehydration, experienced healthcare professionals should perform these challenges in a medical setting with intravenous access and the ability to provide rapid fluid resuscitation. Treatment with a single dose of methylprednisolone is recommended for severe reactions. Routine treatment with antihistamines or epinephrine is not recommended as they do not reduce emesis or lethargy, but a recent report demonstrated a prompt response to treatment with ondansetron in patients with acute FPIES. Accidental ingestions resulting in a reaction often require trips to the emergency department for fluid resuscitation. Providing families with a letter to give to urgent care staff describing the presentation and management of FPIES helps avoid misdiagnosis and reduces the time to provision of optimal therapy.
Management of FPIES
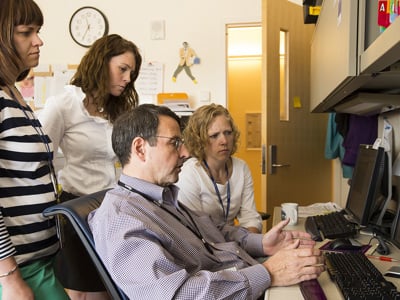
Management of infants with multiple food FPIES often presents a challenge that is best addressed with assistance from other care providers such as an allergist, a gastroenterologist, a dietitian, a feeding therapist and occasionally a psychologist. Input from these specialists aids in ensuring optimal nutrition while on the required elimination diet.
Specialists can provide strategies that reinforce feeding and oral skills infants and children require to help them overcome feeding difficulties caused by unpleasant feeding experiences. Fortunately, the prognosis is excellent as most children outgrow their FPIES within several years.
Contact us
Call our Allergy and Immunology Center at 720-777-2575 or for referrals, contact us through OneCall at 800-525-4871.



 720-777-0123
720-777-0123